AI in Healthcare Examples in the US & Europe That Save Lives
AI in Healthcare Examples in the US & Europe That Save Lives
AI in Healthcare Examples in the US & Europe That Save Lives
AI in healthcare examples already saving lives include tools that detect cancers earlier on medical images, predict sepsis and ICU deterioration, and triage high-risk patients faster in emergency departments across the US, UK and EU. When these supervised machine-learning systems are integrated into EHR and imaging workflows and deployed under HIPAA, GDPR and EU AI Act safeguards, they support clinicians’ decisions rather than replace them, improving outcomes while staying compliant.
Introduction
AI in healthcare examples are no longer “future use cases” on a slide deck they are running right now in hospitals from New York and Boston to London, Berlin and Stockholm. Predictive models are watching vital signs for signs of impending sepsis, computer vision is flagging suspicious breast lesions, and triage tools are pushing the sickest patients to the front of the queue.
In the US, federal data suggests adoption of predictive AI in hospitals rose from roughly 66% in 2023 to around 71% in 2024 as more systems integrated models into their electronic health records (EHRs). Across Europe, the European Commission now treats most medical AI as “high-risk”, reflecting both its impact and the need for tight controls.
This article walks through concrete, life-saving AI in healthcare examples in the US, UK, Germany and wider EU and what it actually takes to implement them safely.
AI in Healthcare Examples: Why They Matter Now
Today’s most impactful AI in healthcare examples include early cancer detection from medical imaging, machine-learning models predicting sepsis and ICU deterioration, and triage tools that prioritise high-risk patients in emergency departments across the US, UK and EU. These use cases matter because minutes and hours can make the difference between full recovery, long ICU stays or death.
What We Mean by AI, Machine Learning and “Real-World” Healthcare Use Cases
When we talk about AI in healthcare, we mostly mean supervised machine learning: models trained on historical patient data to predict a diagnosis, risk or next best action. In practice, this spans:
Imaging and diagnostics CNN-based tools reviewing X-rays, CT, MRI and pathology slides.
Time-critical prediction models that estimate a patient’s risk of sepsis, cardiac arrest or ICU deterioration hours before standard scores.
Digital health & telemedicine remote monitoring apps, virtual wards and home-based care programmes.
Administrative automation scheduling, coding, documentation and prior authorisation workflows.
In this guide, the focus stays on real deployments in US, UK and EU hospitals not just lab prototypes.
How AI Is Already Changing Outcomes in US, UK, German and EU Hospitals
Across the Atlantic, adoption is uneven but accelerating:
A US study found that hospitals using AI sepsis prediction tools saw reductions in in-hospital mortality of roughly 20–40% in some deployments.
Analysis of AI in sepsis management suggests that earlier detection using ML can significantly cut sepsis-related mortality and ICU length of stay.
A data brief from US health IT authorities reported that predictive AI in hospitals increased from about two-thirds of hospitals in 2023 to just over 70% in 2024.
In the UK, the NHS AI Lab is funding dozens of projects, from cancer imaging to skin lesion triage and digital teledermatology.
In Germany and wider EU, university centres such as Charité Berlin and EIT Health-backed pilots are running CE-marked tools under MDR/IVDR.
Behind the headlines, these systems are being integrated into Epic and Cerner EHR workflows, deployed on AWS, Azure or Google Cloud in HIPAA/GDPR-ready regions, and wrapped with strong clinical governance services Mak It Solutions often helps architect for regulated sectors like healthcare and fintech. (Mak it Solutions)
3 Life-Saving AI in Healthcare Examples at a Glance
Three of the most impactful AI in healthcare examples today are: early cancer detection from medical imaging, machine-learning models predicting sepsis and ICU deterioration, and triage tools that prioritise high-risk patients in emergency departments. In each case, AI augments clinicians by surfacing hidden risk earlier and more consistently than traditional rules-based scores.
Life-Saving AI in Healthcare Examples
Three practical examples of AI saving lives in healthcare are: scanning X-rays and MRIs for early cancers, flagging sepsis hours earlier than traditional scores, and triaging high-risk patients in emergency rooms so they are treated before deterioration.
Early Disease Detection with AI in Medical Imaging
The most mature AI in healthcare examples involve radiology and pathology:
In New York and Boston, academic medical centres use AI to flag subtle lung nodules on CT scans or microcalcifications on mammograms that human readers might miss when fatigued.
AI tools help estimate malignancy risk scores, prompting earlier biopsies or follow-up imaging.
In NHS England, pilots supported by the NHS AI Lab are using deep learning models to assist with breast cancer screening, stroke imaging and CT analysis helping to manage radiologist shortages while maintaining safety.
In Germany, university hospitals in Berlin and Munich are deploying CE-marked imaging AI under MDR, often hosted in German data centres to meet DSGVO/GDPR and data residency expectations.
These systems don’t “diagnose on their own”; they prioritise and highlight images, suggest probability scores, and integrate into PACS so radiologists stay in the loop.
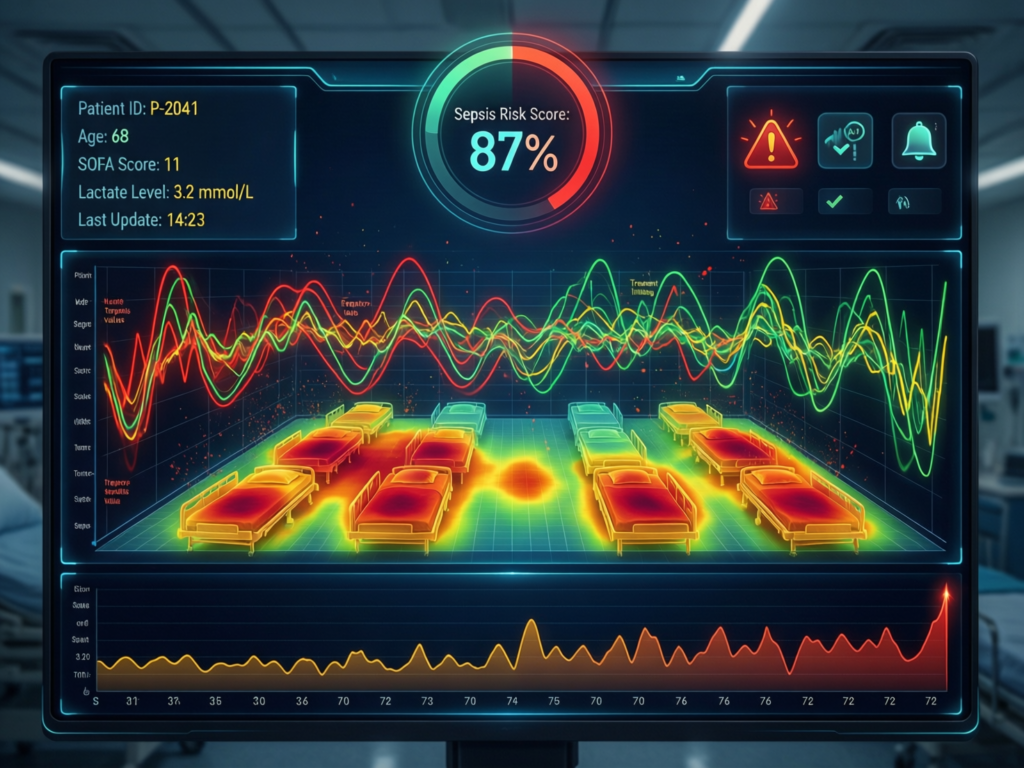
Machine Learning Models Predicting Sepsis and ICU Deterioration
Sepsis is one of the leading causes of hospital mortality worldwide, and minutes matter. AI is now being used to watch continuously for risk:
In multi-site US hospital studies, AI sepsis prediction algorithms integrated with EHR data have been associated with roughly 17–40% reductions in sepsis mortality and shorter length of stay.
German and broader EU ICUs are piloting models that combine vital signs, lab results and ventilator settings to predict clinical deterioration or antimicrobial resistance patterns within hours instead of days. (Healthcare in Europe)
Under the hood, many of these are gradient-boosting or ensemble models trained on large retrospective datasets, or deep learning models that combine structured EHR data with free-text notes. The clinical payoff is straightforward: earlier antibiotics, earlier escalation to ICU and tighter fluid management.
AI Triage Systems Reducing ER Wait Times and Avoidable Admissions
Emergency departments in San Francisco, Houston and across Europe are under constant pressure. AI triage and digital front doors are emerging to help:
US health systems are using symptom-checker apps and nurse decision-support tools that score acuity, suggest investigations and route low-risk patients to “hospital at home” or urgent care.
In the UK, NHS projects are testing AI-assisted symptom checkers and remote monitoring to keep people out of A&E and reduce waiting lists, complemented by self-triage tools evaluated against NHS 111 Online. (Cureus)
In France, the Netherlands and Sweden, telemedicine providers combine smartphone apps, video consultations and AI-based risk scoring to decide who can stay at home with monitoring devices vs who needs a physical exam.
The target outcomes are shorter door-to-doctor times, fewer avoidable admissions and safer use of virtual wards especially for patients with chronic conditions.
Real-World AI in Medicine.
Beyond imaging and ICU alerts, AI supports clinicians with decision support systems, predicts readmissions, powers telemedicine follow-up and automates repetitive administrative work in hospitals across the US, UK and Europe.
Clinical Decision Support and Predictive Analytics for Patient Outcomes
Hospitals are building or buying clinical decision support systems using AI to answer questions such as
What is this patient’s 30-day readmission risk?
Which heart failure patients in Manchester or Munich are most likely to decompensate?
Which oncology patients in Paris or Amsterdam might benefit from a specific targeted therapy?
These models often use gradient boosting or random forests trained on historical outcomes and are surfaced inside Epic or Cerner as risk scores, colour-coded lists or personalised care-plan suggestions.
AI in Digital Health and Telemedicine for Follow-Up Care
AI is also quietly powering digital health and telemedicine.
Remote monitoring kits for older adults in London, Stockholm and Hamburg stream vital signs to the cloud; models detect patterns suggesting falls, heart failure exacerbations or infections.
Chatbots and digital coaches help patients post-discharge to manage medications, wound care and symptoms, escalating to nurses when risk crosses a threshold.
In the EU, programmes funded by EIT Health and national ministries are using AI to prioritise which teleconsultation queues should be reviewed first.
This is where Mak It Solutions’ experience with mobile app development and data platforms becomes crucial secure APIs, low-latency analytics and cross-platform apps matter as much as the ML itself.

Administrative and Workflow Automation in Hospitals
Finally, some of the biggest ROI sits in what patients never see.
Automated coding suggestions, denial prediction and documentation summarisation.
AI that drafts clinic letters or insurance forms for clinicians to edit.
Prior authorisation tools that check clinical criteria and flag missing documentation.
One report suggests that around a quarter of US hospitals already use AI-driven predictive analytics, often starting in revenue cycle and operations before moving to clinical use cases.
These workflow wins free up physicians and nurses to focus on patients, not paperwork especially when combined with business intelligence and analytics services to track impacts.
Machine Learning in Healthcare Examples: How the Technology Works
Most life-saving AI in healthcare is powered by supervised machine learning models trained on historical patient data such as convolutional neural networks for image recognition and gradient-boosting models for risk prediction integrated into existing EHR and imaging workflows.
The ML Models Behind Life-Saving Use Cases
At a high level.
Convolutional Neural Networks (CNNs): excel at pattern recognition in images (X-ray, CT, MRI, digital pathology). They learn features like edges, textures and shapes associated with disease.
Gradient boosting / tree ensembles: strong for tabular EHR data (labs, vitals, medications). They capture non-linear interactions, ideal for sepsis risk or readmission models.
Recurrent / transformer models: good for time-series vital signs or free-text notes.
In US ICUs, for example, CNNs can screen chest X-rays for pneumothorax while an ensemble model watches vitals and labs for sepsis risk; the combination drives nuanced, early alerts.
Data Pipelines, Cloud Platforms and EHR Integration
The technology stack matters as much as the algorithm:
Data pipelines pull from EHRs (Epic, Cerner), PACS, lab systems and monitoring devices into a secure data lake or warehouse.
Many hospitals use AWS, Microsoft Azure or Google Cloud healthcare-ready regions with private networking, encryption and audit trails.
In the EU and UK, GDPR and national data residency rules steer workloads into specific regions (e.g., Frankfurt, London, Paris) or into on-prem Kubernetes clusters.
Mak It Solutions often helps design these cloud architectures from landing zones and VPCs to CI/CD pipelines so healthcare teams can plug in AI tools without reinventing cloud engineering. (Mak it Solutions)
Measuring Impact: From AUC to “Lives Saved” and Cost Avoidance
ROC AUC and F1 scores look impressive, but hospital leaders care about.
Lives saved and complications avoided for example, a sepsis AI that reduces mortality by about 20% at Johns Hopkins and 17% at UC San Diego.
Operational impact ICU days reduced, ER throughput improved, radiologist reporting times cut.
Financial impact lower readmissions, shorter stays, fewer penalties from CMS or insurers.
A robust implementation includes before/after studies, bias audits and continuous model monitoring, not just a “go live” date.
Implementing AI in Hospitals in the US, UK and EU
Hospitals that successfully adopt AI start with a clearly defined use case, partner with compliant vendors, run small pilots in one department, measure clinical and operational impact, and only then scale across sites.
Choosing the Right Use Case and Healthcare AI Vendor
Good starting points include
Painful bottlenecks (e.g., stroke imaging turnaround, sepsis in ICUs, ER overcapacity).
Clear metrics (mortality, length of stay, readmission, wait times).Data availability and quality.
When comparing vendors in New York, London or Berlin, check:
Integration with Epic/Cerner and your PACS.
Cloud architecture (AWS/Azure/GCP), regions and data residency.
Security credentials (SOC 2, ISO 27001) and experience with HIPAA, GDPR, BaFin or NHS requirements.
Mak It Solutions often supports clients with multi-cloud assessments for example, whether to host regulated AI workloads on AWS, Azure or Google Cloud in US vs UK vs Germany/EU. (Mak it Solutions)
From Pilot to Production
A strong AI pilot
Runs in one unit (e.g., a single ICU in Boston or a radiology department in Manchester).
Has a named clinical champion and a multidisciplinary steering group.
Keeps humans in the loop: alerts are advisory, not auto-orders.
Change management, training and governance are as important as the model exactly the kind of human-centred change management Mak It Solutions already delivers for cloud and SaaS transformations.

Cloud-Based AI, On-Prem and Hybrid Approaches in Different Regions
Patterns by GEO.
US
Many providers use cloud-native AI platforms in HIPAA-ready regions, with BAAs in place and PHI tokenisation for secondary analytics.
UK
NHS trusts often choose hybrid models: local data centres plus NHS-approved cloud providers, ensuring UK-GDPR and NHS DSPT compliance.
Germany / wider EU
Strong preference for EU data residency (Frankfurt, Berlin, Paris regions) and data-minimised cross-border transfers under GDPR and Schrems II.
Cloud cost and performance are key which is why teams pair AI planning with cloud cost optimisation and shadow IT governance.
Compliance, Ethics and Regulation for Healthcare AI
In the US, life-saving AI tools must comply with HIPAA and security frameworks like SOC 2; in the EU, they are treated as high-risk systems under the EU AI Act and GDPR; and in the UK they must align with UK-GDPR, NHS AI standards and ICO guidance on automated decision-making.
Note
This article is for general information only and does not constitute legal, regulatory or medical advice. Healthcare organisations should consult qualified counsel and clinical leaders before making decisions.
US Landscape
In the United States:
HIPAA sets national standards for protecting PHI, enforced by HHS and OCR.
AI vendors hosting PHI must sign Business Associate Agreements (BAAs).
SOC 2 and sometimes PCI DSS (for payment flows) provide additional security assurance.
Hospitals should ensure AI platforms provide audit logs, role-based access control, encryption and clear incident response procedures.
EU and Germany.
In the EU and Germany:
GDPR/DSGVO governs processing of personal data, including health data, and mandates lawful bases, minimisation and strong data subject rights.
The EU AI Act treats most medical AI as high-risk, layering additional requirements (risk management, high-quality datasets, transparency and human oversight).
Tools that qualify as medical devices must also comply with MDR/IVDR and, in Germany, guidance from BfArM and national data protection authorities.
Implementation timelines for some high-risk AI provisions may stretch into 2027, but regulators are clear: safety, transparency and accountability are non-negotiable.
UK Context: UK-GDPR, NHS, NHSX Standards and ICO Guidance
In the UK.
UK-GDPR and the Data Protection Act set similar principles to the EU GDPR.
The ICO provides detailed guidance on AI, automated decision-making and DPIAs.
The NHS AI Lab and NHS AI standards set expectations around safety, explainability and equity, especially for tools deployed inside the NHS.
Any AI vendor pitching to NHS trusts should be ready to show.
Clear clinical evaluation.
Bias and fairness assessments.
Interoperability with NHS infrastructure and NHS England guidance.
How to Launch Life-Saving, Compliant AI in Your Healthcare Organization
Healthcare providers in the US, UK and EU can safely implement AI by starting with a narrow, high-value use case, partnering with compliant vendors, piloting in one unit, rigorously measuring clinical outcomes and equity, and only then scaling under strong data-governance and regulatory frameworks.
Assess Data, Risks and Clinical Priorities
Map your priorities
Identify 2–3 use cases with clear clinical and operational value (e.g., sepsis prediction in Houston, stroke imaging in London, triage support in Berlin).
Audit data and integration
Understand what’s available in your EHR, PACS and monitoring systems; assess data quality, coding standards and interoperability gaps.
Build a risk and governance register
Document clinical, ethical, cybersecurity and regulatory risks; define your AI risk committee, DPO and clinical safety officer roles.
Select Partners, Pilot AI and Prove Outcomes
Select partners and architecture
Decide on build vs buy; evaluate vendors’ technical stack (AWS/Azure/GCP, on-prem, hybrid), security posture and regional hosting.
Run a structured pilot
Launch in one ward or site; keep AI as decision support; capture baseline and post-implementation metrics; involve frontline clinicians in design.
Prove outcomes and equity
Evaluate mortality, LOS, readmissions and ER throughput; analyse performance across demographic groups; refine thresholds and workflows.
Scaling Across Sites in the US, UK, Germany and Wider Europe
Once the pilot is proven:
Roll out to additional hospitals in your US network, then adapt to NHS or German hospital contexts as appropriate.
Establish cross-border data-sharing agreements that respect GDPR, UK-GDPR and local rules.
Treat AI platforms like any other critical clinical system: versioning, SLAs, monitoring and continuous validation.
This is where a partner like Mak It Solutions already helping organisations with shadow IT governance, cloud landing zones and AI-ready architectures can accelerate the move from pilot to safely scaled production.

Key Takeaways.
Imaging AI
Helps radiologists and pathologists in New York, London and Berlin spot cancers and critical findings earlier, reducing delays to treatment.
Sepsis and ICU prediction models
Give clinicians extra hours to act in US, German and EU hospitals, cutting mortality and ICU length of stay.
Triage and remote monitoring tools
Keep emergency departments flowing and support hospital-at-home and virtual wards in the UK, France, Netherlands and Sweden. (Cureus)
Decision support, telemedicine and admin automation
Free up scarce clinicians while maintaining safety and compliance in systems like Medicare, NHS and BaFin-regulated providers.
Compliance by design
HIPAA, GDPR/DSGVO, EU AI Act, UK-GDPR, NHS AI standards and PCI DSS where payments apply is now essential to build trust with regulators and patients alike.
Questions to Ask Any Healthcare AI Vendor Before You Sign
Before you commit budget and clinical workflows, ask.
Clinical evidence
In which US, UK or EU hospitals has your model been deployed, and what outcomes did you measure?
Bias and equity
How have you tested for bias across age, sex, ethnicity and socio-economic groups, and what happens if we find issues?
Integration
How do you integrate with our EHR (Epic/Cerner), PACS and cloud stack (AWS/Azure/GCP)?
Compliance
How do you meet HIPAA, UK-GDPR, GDPR and EU AI Act requirements, and can we see DPIAs, security reports and CE/FDA clearances?
Ownership & governance
Who owns the model, data and IP, and how are updates, retraining and monitoring handled?
If a vendor can’t answer these clearly, they’re not ready for your patients.
If you’re planning to move from AI slide decks to real, life-saving implementations in your hospital network, you don’t have to design everything from scratch. Mak It Solutions can help you map regulations, design cloud and data architectures, and build the web, mobile and analytics platforms your AI tools depend on whether you operate in the US, UK, Germany or wider Europe.
Reach out to Mak It Solutions to book a discovery workshop: we’ll assess your data, shortlist high-value AI in healthcare examples for your context, and design a compliant roadmap from first pilot to multi-site rollout. ( Click Here’s )
FAQs
Q : Is AI in healthcare allowed under GDPR and the EU AI Act, or is it considered too risky?
A : Yes, AI in healthcare is allowed under GDPR and the EU AI Act, but most clinical tools are treated as high-risk systems. That means they must meet strict conditions: lawful processing of health data under GDPR, strong security, risk management, human oversight and transparency about how decisions are made. Rather than banning AI in hospitals, EU regulators are demanding better documentation, monitoring and alignment with MDR/IVDR for medical devices. If your data governance and vendor due diligence are strong, AI projects can be both compliant and clinically impactful.
Q : Will AI replace doctors and nurses, or mainly support them with decision-making?
A : Current deployments in New York ICUs, NHS hospitals and German university centres all position AI as decision support, not a replacement for clinicians. AI is good at spotting patterns in huge datasets and staying vigilant 24/7, but it lacks context about patients’ values, complex co-morbidities and social circumstances. Regulators like HHS, NHS England and EU bodies expect a “human in the loop”, especially for high-risk decisions, and the most successful projects keep physicians and nurses in charge while using AI to reduce missed risks and cognitive load.
Q : How accurate are AI diagnostic tools compared with human clinicians in real hospital settings?
A : Accuracy varies by tool and setting, but many FDA- or CE-marked imaging models reach radiologist-level sensitivity for specific tasks, such as detecting lung nodules or breast lesions.However, performance in real-world hospitals can be lower than in ideal test datasets due to data drift and workflow issues. That’s why responsible hospitals run local validation, monitor ongoing performance, and treat AI outputs as one more input into a clinician’s judgment not the final answer.
Q : What data do hospitals need to start training or using machine learning models safely?
A : For most machine learning in healthcare examples, hospitals need: high-quality, well-coded EHR data (diagnoses, procedures, meds), time-stamped vitals and labs, and outcome labels (e.g., sepsis, ICU admission, mortality). Imaging or waveform models also need well-annotated scans or signals. You don’t have to centralise everything in one place, but you do need clear data governance, de-identification for model training, and technical pipelines that respect HIPAA, GDPR/UK-GDPR and local regulations.
Q : How can smaller clinics or practices use AI in healthcare without a big data science team?
A : Smaller clinics in Manchester, Austin or Hamburg usually buy, not build. They start with:
Cloud-hosted AI-enabled EHR features (e.g., risk flags, note summarisation).
Imaging tools from established vendors that integrate into existing PACS.
Telemedicine platforms with built-in triage and decision support.
The key is choosing vendors with strong compliance, clear pricing and good support, and working with implementation partners (like Mak It Solutions) for integration, training and change management. You can get real benefits from AI in scheduling, documentation and patient engagement long before you hire an in-house data science team.


